Prior to prohibition, cannabis was revered as a bountiful plant resource with thousands of industrial, nutritional and healing applications, some dating back as far as 4000 B.C. By the early 1930s, marijuana was readily available and frequently prescribed to treat a variety of common ailments. No sooner than Popular Mechanics published a cover story predicting that hemp would become a billion dollar industry, the infamous “Reefer Madness” campaign sufficiently demonized its marijuana cousin and the Tax Stamp Act of 1937 set the stage for prohibition of all forms of cannabis. Legal marijuana had already become a distant memory by the time Congress passed the Controlled Substances Act of 1971, which added marijuana and hemp to the DEA’s list of Schedule 1 narcotics. The ensuing War On Drugs provided fertile ground for the pharmaceutical industry to make a killing on synthetic prescription drugs, some of which have proven to be far more dangerous than marijuana.
Nearly 80 years and several generations later, cannabis is re-emerging from the shadows of prohibition with renewed acceptance and potential to redefine modern medicine for the next generation. However, people raised on propaganda spawned by the Reefer Madness and War On Drugs eras have been slow to embrace cannabis as a viable alternative to its popular, but deadly, pharmaceutical replacements.
Finding anyone old enough to remember using medicinal cannabis before prohibition began would be a tall order. Ironically, a few daily doses of a cannabis concentrate might very well help them to remember – and effectively render an assortment of prescription pills for memory loss and other age-related ailments obsolete.
Finding peer-reviewed clinical studies to validate such a presumptuous postulation might also be a tall order. In all likelihood there aren’t many – if any – yet. However, personal experience and some very compelling anecdotal evidence has this author convinced that cannabis is a far safer alternative to some of the most dangerous pharmaceuticals too commonly prescribed to treat elderly patients.
A Personal Case Study
On July 25th, 2016, my father was admitted to a San Diego hospital after a fall caused by a severe drop in blood pressure. Several days later, he began experiencing tremors, hallucinations and severe agitation. Before long, the doctors realized that he was suffering from delirium tremens (DT) caused by withdrawal from a combination of drugs prescribed for existing medical conditions and alcohol – his daily escape from the haunting, post-trauma memories of the Vietnam War. Within four days of admission, he had slipped into an obtunded state, a twilight form of coma, sustained by a feeding tube and intravenous fluids.

August 25: Several days after emerging from a semi-comatose state, diagnosed with Wernicke’s encephalopathy, a reversible condition
When he regained consciousness four weeks later, his cognition and physical ability to function were severely limited. He was assigned a 24-hour sitter to prevent him from pulling his feeding tube and impulsively trying to roll out of bed.
His initial diagnosis was Wernicke’s encephalopathy, an often-reversible form of dementia caused by DT. We were optimistic when he began to relearn basic functions like swallowing, speaking and moving limbs on command with regimented physical, occupational and speech therapy.
Since hospitals are notorious for spreading infectious disease, doctors were eager to transfer him to a skilled nursing facility for rehabilitation. Once they felt confident that he was capable of remaining alone without a sitter for 24 hours, they would transfer him.
Anticipating it would take several days, and knowing he was on the mend, I decided to return to work in Arizona. A day later, I received a call that he had already been moved. That was on September 9th.
Believing that my father had been in good hands and receiving rigorous physical therapy, I didn’t return to San Diego until four days later. I was devastated to find that he had slipped back into semi-conscious state. Therapy had been impossible since he had no control over his movements and was unable to respond to simple commands.
What we didn’t know until later is that they had drugged him with Ativan (a benzodiazepine sedative) and Haldol (an anti-psychotic) in order to keep him still enough to be unattended for the required 24-hour duration. Overnight, all of the progress he had made was reversed. When he was awake, hallucinations obscured his reality. Convulsive tremors shook his body every 10 minutes. Medication he was receiving intravenously didn’t help; they seemed to be killing him. The facility doctor disagreed with our assessment, but offered no solution other than to keep him drugged.
We had an ambulance take him to the San Diego Naval Hospital for a second opinion. Blood work revealed he was severely malnourished and dehydrated. He had a fever of 102F, which we learned was due to an untreated e-coli infection. By then, he had lost 27 percent of his body mass. A speech therapist determined that he would likely never recover the ability to swallow on his own. He was finally diagnosed with degenerative neuropathic encephalopathy with multi-system atrophy. The prognosis was bleak, organ failure within two weeks at the most. Doctors recommended hospice.
The Fight of His Life
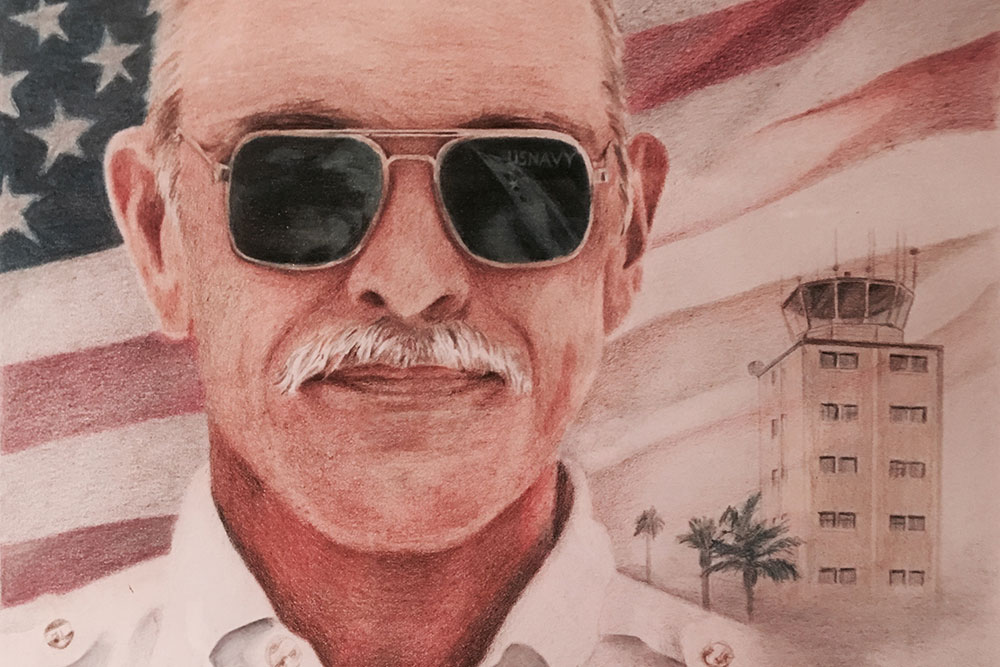
It was inconceivable to me my father, an energetic, proud Navy veteran who had been living independently, driving his own car, flying his own plane and traveling the world with his fiancé Ann just weeks before, wouldn’t recover. Even in his fragile state, he began to show signs that he wanted to live. Failure was never an option for him, so I wasn’t about to give up hope. At my request, the doctors stopped all medication. I worked with him to get him to squeeze my hand. When I dipped a swab in apple juice to moisturize his mouth, I saw him swallow. When I mentioned his grandson, he tried to smile.

September 11: Diagnosed with degenerative neuropathic encephalopathy with multi-system atrophy and given two weeks to live.
Seeing the slightest improvement since his medicine was discontinued had me convinced that drugs had caused his latest regression. I decided to do some research and learned that my supposition wasn’t off base. According to recent studies, benzodiazepines and anti-psychotics commonly prescribed for anxiety, confusion and combative behavior, can be harmful to elderly patients, especially those with a history of alcoholism, dementia or a traumatic brain event. Other studies prove that cannabis is a much safer alternative.
Having written about cannabis since 2010, I have received first-hand testimony from mothers, veterans and cancer patients who have witnessed miraculous healing with cannabis when conventional pharmaceuticals have failed. Why not my father?
When All Else Fails
As is the case with many people my father’s age, Reefer Madness had shaped his perception. He never condoned any use of marijuana – in fact, he thought I was crazy for writing about it. Ironically, cannabis could be his last hope for survival. Faced with no other alternative, I decided to forego his permission and ask him for forgiveness later. After all, the decision was up to me; he entrusted me with durable power of attorney for his healthcare in the event he couldn’t make such decisions for himself.
Instead of calling hospice, we transferred him to a post-acute care facility and signed an order refusing all pharmaceuticals. Under the radar of the facility’s nursing staff, I immediately began giving him a dropper-full of potent hemp-derived CBD oil several times a day. The results were nothing short of astonishing:

Albert Jay Shower talking with his son and grandson two weeks after receiving his first dose of CBD — clear signs that he was on the road to recovery and defying a devastating prognosis
Week 1 – He pulled out his feeding tube, began swallowing on his own and his tremors disappeared;
Week 2 – He sat up on his own, began to talk and could swallow pureed food;
Week 3 – He began feeding himself and was able to stand up with a therapist;
Week 4 – He took his first steps in physical therapy, tied his own shoes and began speaking intelligibly;
Week 5 – He could read, write his name and was making plans for a vacation in New Zealand.
A Reversal of Fortune
With toxic drugs out of his system, the CBD oil was working wonders, but not without unintended consequences. As he regained his strength, he became impatient and desperate to do everything on his own. With nonstop facility noise and a snoring roommate, he had trouble sleeping through the night. He tried to get out of bed without assistance, but fell to the ground each time. During daylight hours, he’d attempt to get out of his wheel chair to rush to the bathroom but was restrained by nurses who didn’t realize the urgency. The indignity of losing control of himself made him angry, but the doctors attributed his “combative” behavior to dementia-related anxiety and agitation.

October 11: Working with an occupational therapist prior to receiving Ativan for “agitation”
Since the facility didn’t have adequate staff to supervise his movements to keep him from falling, the administrators gave us an ultimatum: either we authorize sedatives to chemically restrain him or move him to another facility. Realizing it would take time to find a new facility to accommodate his needs, we reluctantly agreed to sedation under the condition that a minimal dose would be administered, and only if needed.
Within two hours of receiving his first new dose of Ativan, he returned to an obtunded state, unable to sit up, eat, speak or participate in any therapy at all. The convulsive tremors and hallucinations returned. It took nearly 48 hours for a single dose to wear off at which time he became confused, agitated and combative to the point that the nurses insisted upon giving him another dose.
A Vicious Cycle
Upon further investigation, I learned that some of the side effects of benzodiazepines like Ativan include short-term memory loss, hallucinations, tremors and combative behavior as the drug wears off. It’s a vicious cycle – the behavior it is prescribed to control is the very behavior it causes once it wears off. Although the dose he received was considered to be low, his body wasn’t tolerating it. Ativan was not only obstructing his recovery, it was taking him down a spiral of dependency with zero upside.
Unfortunately, finding a state-licensed skilled nursing facility willing to administer cannabis is next to impossible, even in California, which has plenty of health practitioners well-versed in cannabis and a pending legalization measure favored to win the popular vote.
I began calling upon my contacts in the cannabis industry for advice. It seems others have experienced the same issues with aging parents, sick children and their own conditions. Institutional medical facilities that would permit medical marijuana treatment simply don’t exist due to Federal law and the absence of policy doctrine in states where medical marijuana is legal. Most medical doctors won’t get involved for fear of losing their DEA license to practice medicine.
Our only option was to find a private group home willing to allow the unconventional treatment. We decided to move him to Arizona where I have resources to ensure he can receive the holistic medicine and care he needs.
Anecdotal Evidence: A New Lease On Life

December 1st: On CBD with zero Ativan for 5 weeks, working with therapists 6 days a week
The move took place on October 30th when, for the first, only and last time, I actually requested that nurses at the California facility sedate my father to prepare him for the six-hour drive to Arizona. It took five days to clear the Ativan out of his system and the miraculous recovery began anew.
On the fourth night of November, for the first time since July 25, my father stood up and walked across a room without any assistance.
Since then, we have retained a cannabis-friendly internal medicine specialist to serve as his new primary care physician on a concierge basis. With his help, we registered my father as a medical marijuana patient and began whole plant cannabis treatment. My father still has a long recovery ahead and it’s uncertain whether he can fully regain his independence. But there is no doubt that cannabis is working to improve his odds of resuming a better quality of life.
Editorial Footnote: February 9, 2018
Since this article was written in 2015, Albert “Jay” Shower has been living in comfort, free from the debilitating tremors of Parkinson’s and without any pharmaceutical restraints because he had access to the healing power of cannabis. It is with great sadness that we report that he is preparing for his final flight with angels, but we are in gratitude for his life and salute him for his service to our country.
Veterans who sacrifice so much to protect our freedom deserve the freedom to choose their form of treatment without threat of losing their dignity or quality of care from the VA. If you are a veteran who has found healing with cannabis and would be willing to share your experience so that other veterans can discover an alternative to help them cope with PTS, please contact us and let us know.